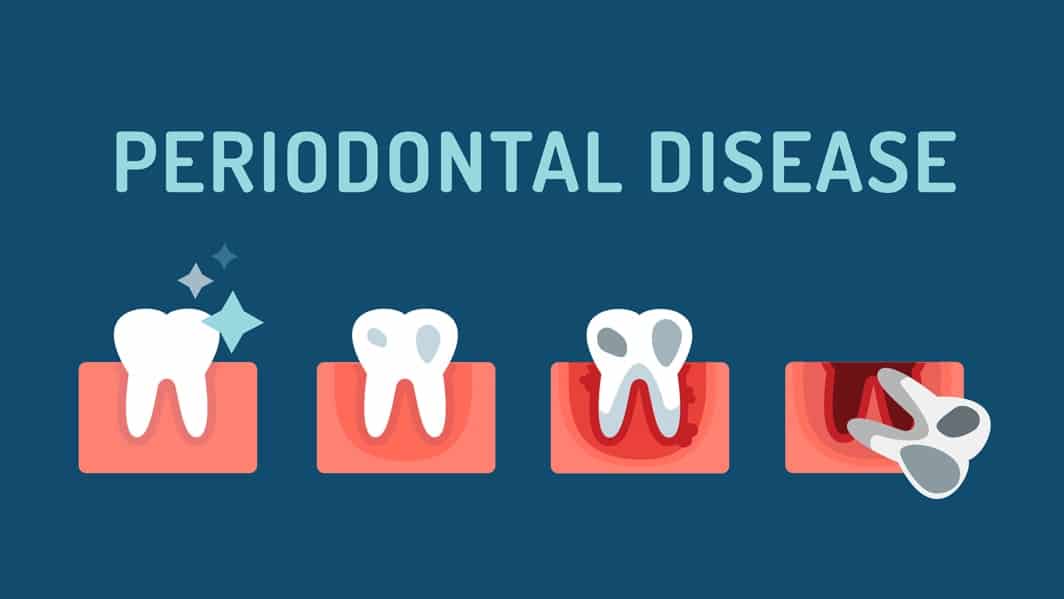
Gum disease–also known as periodontal disease and periodontitis–is a common occurrence in people of all ages. It begins as gingivitis, which results from the bacteria in plaque building up and causing gum inflammation. Not all gingivitis progresses to periodontitis thanks to prompt dental treatment. When progression does occur, however, tooth loss is a very real possibility. Left untreated, periodontitis causes the bone and connective tissue that anchor teeth in place to slowly break down. In fact, gum disease is the leading cause of tooth loss in adults.
Causes of Gum Disease
Plaque is the primary culprit behind periodontal disease. However, there are many factors that can make a person more susceptible to gum disease, including:
- Insufficient oral hygiene. Because gingivitis is caused by a build up of bacteria in plaque, poor oral hygiene sets the stage for this process to occur. Patients who do not brush their teeth twice a day and floss daily are much more likely to develop gingivitis and ultimately have it progress to periodontitis.
- Certain medications. A common side effect of certain medications is dry mouth. With a decreased saliva flow, patients are more susceptible to gum disease, as saliva helps to protect both the teeth and the gums.
- Hormones. Women may be more likely to develop gum disease due to certain hormonal changes that occur throughout the lifetime, including those changes that occur during puberty, pregnancy, menstruation, and menopause. During these times, the gums tend to be more sensitive, thereby increasing the chance of gingivitis developing.
- Genetics. A strong family history of oral health diseases might make patients more likely to develop gum disease.
- Smoking. It’s no secret that smoking has a number of negative effects on oral health, ranging from halitosis to an increased likelihood of oral cancer. Smokers are also more susceptible to periodontitis because smoking impairs the gum tissue’s ability to repair itself when damaged.
- Health concerns. Certain medical conditions put patients at a greater risk of developing gum disease. Patients suffering from diabetes are more susceptible to infections in general, including gum disease. Additionally, patients with illnesses that suppress the immune system, such as HIV, are also at an increased risk of developing periodontal disease.
Symptoms of Gum Disease
Only your dentist can definitively diagnose gum disease, but there are some common symptoms that might signify a potential problem:
- Bleeding gums. One of the most common symptoms of early gingivitis is bleeding gums. If your gums bleed regularly while you’re brushing your teeth, it’s time to visit your dentist.
- Tender gums. Even if your gums aren’t bleeding, if they’re red, swollen, or tender, you might be suffering from gingivitis.
- Gum recession. If you notice that your gums are receding, or pulling back from the surface of your teeth, periodontal disease is a likely cause.
- Halitosis. While there are many causes of halitosis, persistent bad breath can sometimes be indicative of diseased gums. A chronic foul taste in the mouth should also send up a red flag that a dental check-up is necessary.
- Loose teeth. If your teeth are loose or shifting, you’ve likely progressed beyond gingivitis to periodontitis. Seek dental treatment immediately.
Treatment and Prevention
Treatment for gum disease depends on how far the disease has progressed. Sometimes, your dentist might simply recommend therapies to control bacterial growth. If the disease has progressed significantly, however, surgery to restore diseased tissues might be necessary.
The key to preventing gum disease is controlling plaque. In addition to practicing good oral hygiene– including brushing twice a day and flossing every day– it’s essential to visit your dentist every 6 months for check-ups and professional cleanings. Contact us today to learn how we can help you achieve your healthiest smile.
